What is Epidermolysis Bullosa?
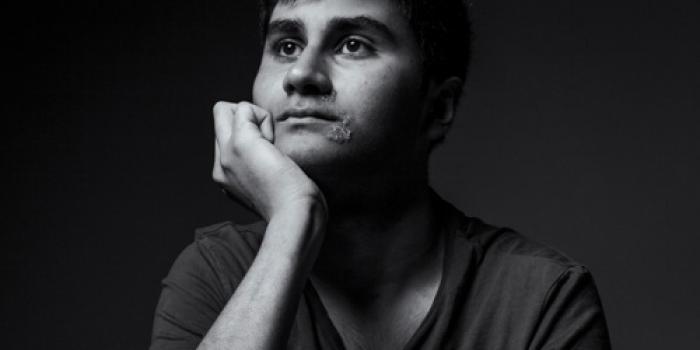
Epidermolysis Bullosa (EB) is a group of rare genetic disorders that cause the skin and mucous membranes to be extremely fragile. Even minor friction, heat, or trauma can result in painful blisters and open wounds.
EB can also affect the mouth, eyes, esophagus, and other internal organs, leading to complications that impact nutrition, mobility, and overall health. The condition varies widely in severity—from mild blistering on hands and feet to life-threatening forms that affect multiple body systems.
There is currently no cure for EB, but symptom management, wound protection, and multidisciplinary care are essential for maintaining comfort and preventing complications. With proper support and expert care, many people with EB lead fulfilling lives despite the daily challenges of the disease.
EB Facts:
Genetic Origin: EB is not contagious. It’s caused by mutations in one of 18 genes responsible for producing structural proteins—such as collagen VII, keratin 5 or 14, and laminin-332—that anchor skin layers together.
Skin Fragility: Without proper anchoring, the skin layers do not hold together as they should. Even minor friction, rubbing, or heat can cause recurrent blisters, tears, and open wounds. Internal systems may also be affected.
Prevalence: Affects 1 in every 20,000 births (~200 children with EB born annually in the United States).
Across All Populations: Impacts all genders and racial/ethnic groups equally.
Living with EB
Living with EB requires meticulous and often time-consuming care. Most people with EB (or their caregivers) follow a strict daily routine of wound inspection, draining new blisters, cleansing skin, applying ointments, and wrapping affected areas with specialized bandages to prevent infection and further injury. There are four major types of EB: EB Simplex (EBS), Junctional EB (JEB), Dystrophic EB (DEB), and Kindler Syndrome. Refer to each EB type in the section below for detailed signs, symptoms, and associated genetic mutations.
For those with severe forms of EB, this process can take hours each day. Tasks many take for granted—like bathing, getting dressed, or eating—can cause blistering. Wounds often heal slowly or not at all, and managing pain is a constant challenge. The condition can also lead to secondary complications, such as infections, chronic anemia, scarring and contractures, which further complicate daily life.
Moreover, EB’s impact extends beyond the skin. It can affect other systems, including the eyes, mouth, and gastrointestinal tract, and may lead to long-term issues like difficulty swallowing, limited mobility and vision problems. Despite these difficulties, individuals and families living with EB show immense strength and resilience as they navigate a condition that touches nearly every aspect of daily life.
Types of EB
There are four major types of EB—EB Simplex (EBS), Junctional EB (JEB), Dystrophic EB (DEB), and Kindler Syndrome—each tied to different gene mutations and the specific layer of skin affected. Symptoms range from chronic blistering to life-threatening complications. Each type of EB includes subtypes, and severity can vary significantly—even among individuals with the same diagnosis.
Refer to each EB type below for detailed signs, symptoms, and associated genetic mutations.
 EB Simplex (EBS)
EB Simplex (EBS)
EBS is the most common type of EB, and affects the upper layers of the skin's epidermis.
Learn More Junctional EB (JEB)
Junctional EB (JEB)
JEB affects where the outer skin (epidermis) and inner skin (dermis) layers connect, in the skin's the basement membrane.
Learn More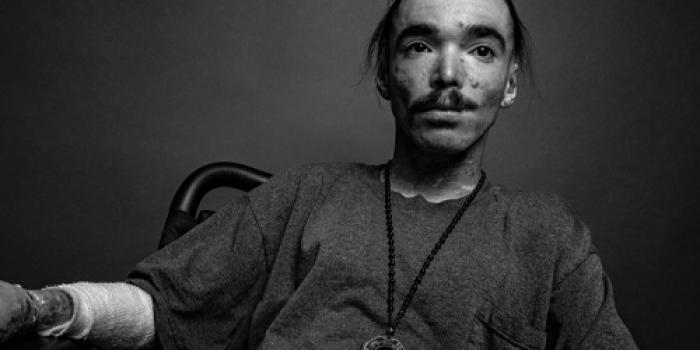 Dystrophic EB
Dystrophic EB
DEB affects the dermis, beneath the basement membrane. This results in blistering in the deeper layers of the skin.
Learn More Kindler Syndrome
Kindler Syndrome
Kindler EB is a rare type of EB that affects multiple layers of the skin, including both the outer skin (epidermis) and inner skin (dermis).
Learn MoreEpidermolysis Bullosa Acquisita (EBA): What is EBA? While similar in appearance, EB Acquisita differs from the genetic forms of EB. It is a rare autoimmune condition, typically developing after age 40, in which the immune system mistakenly attacks type VII collagen (the protein that anchors layers of skin) causing blistering and skin fragility. While there is no cure, there is treatment that focuses on managing symptoms with immunosuppressive or anti-inflammatory medications. People with EBA are typically referred to a rheumatologist. For more information and support, visit: DermNet NZ – EBA Overview.
Diagnosis, Care, and Support
Epidermolysis Bullosa (EB) is typically diagnosed through clinical evaluation and genetic testing. This process helps determine the specific type of EB, which is essential for creating a personalized treatment plan. Symptom management, including proper wound care, pain relief, and nutritional support, is crucial to minimizing complications. A multidisciplinary team is often involved to address the wide-ranging effects of EB.
For additional guidance on diagnosis, treatment, and ongoing care, visit our Getting Diagnosed and Managing EB pages. Visit our Support & Resources section to learn more about our direct services, including one-on-one support, help navigating care, and opportunities to connect with the EB Community and medical professionals.
For more information or if you have any questions, feel free to contact us at:
Email: staff@debra.org
Phone: 833-debraUS (833-332-7287)
Our team is here to support you with any questions or concerns regarding EB diagnosis, treatment, and ongoing care.